By HeadlineNews.News Health Desk
July 5, 2025 | Abuja
Overview of the Controversy
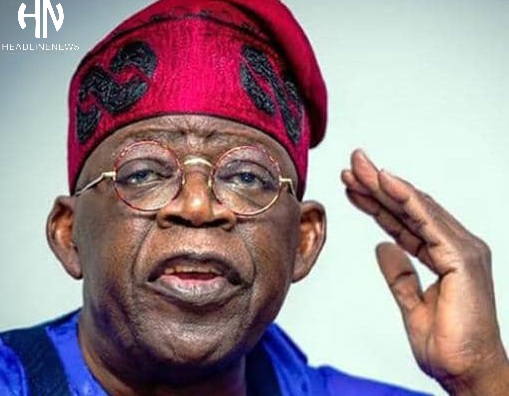
The Nigerian Medical Association (NMA) has sharply criticized the Federal Government’s new Technical Manpower Assistance (TMA) agreement with Saint Lucia, calling it “inexcusable” in light of the poor working conditions at home. The deal, formalized on July 2 during President Tinubu’s tour of the Caribbean, allows Nigerian doctors to serve abroad for two-year terms, including in the Organisation of Eastern Caribbean States (OECS).
NMA Secretary-General Dr. Benjamin Sichey Egbo sharply criticized the timing and terms of the agreement, highlighting alarming disparities in pay and welfare.
Stark Pay Disparities: Who’s Earning What
Location & Annual Pay to Doctors
Saint Lucia Govt.- ₦131.7 million
Nigerian Govt. (for TMA)- ₦40.8 million
Doctors in Nigeria- ₦11.9 million
NMA notes that while the Saint Lucian government pays over ₦131 million annually, Nigeria will pay ₦40.8 million—yet doctors at home earn just ₦11.9 million, excluding hazard allowances. Egbo called the move a glaring example of double standards.
Brain Drain & Healthcare Crisis
- Nigeria is in the throes of a massive medical brain drain:
- Over half of licensed Nigerian doctors practice abroad.
- Around 727 doctors emigrated to the UK between December 2021 and May 2022.
- Nearly 57,000 nurses left between 2017 and 2022.
- The physician-to-patient ratio in Nigeria hovers at approximately 1:5,000, far below the WHO minimum of 1:600.
This exodus has triggered overwork, burnout, medical negligence, and worsening health outcomes, particularly in maternal and mental health.
Living Through Hardship: Doctors’ Plight in Nigeria
- The NMA underscored systemic neglect:
- Chronic delays in MRTF disbursements
- Non-implementation of CONMESS salary structure
- Withheld hazard allowances despite workplace risks
- Unsafe environments and high-stress
NMA has issued a 21-day ultimatum for the reversal of the NSIWC circular and fulfillment of prior welfare agreements, or risk nationwide industrial action.
Root Causes & Historical Context
Nigeria has battled brain drain since the 1980s. Investment in medical education, estimated at US$21,000–51,000 per doctor, is regularly lost to emigration. The medical workforce crisis is exacerbated by:
- Low healthcare budget (≈ 4–6%, below AU’s 15% target).
- Poor working conditions, infrastructure decay, and political neglect.
- Security concerns, inflation, and broader socio-economic pressures.
Global Voices on Brain Drain
> “Wealth lies not just in training professionals, but in keeping them.”
— Ngozi Okonjo‑Iweala, WTO Director‑General.
> “Exporting skilled labor for prestige while ignoring domestic health needs is moral bankruptcy.”
— Dr. G. Fraser, MFR, The National Patriots, Governance & Public Policy Analyst
Analysis: Diplomacy vs Domestic Priority
The TMA deal aimed to strengthen South-South ties and broaden Nigeria’s expatriate footprint. However, critics argue:
- Deploying overstretched doctors abroad amid acute local shortages could deepen healthcare collapse.
- Payment gaps suggest Nigeria is offloading costs while undermining doctors’ livelihood at home.
- The move risks becoming symbolic diplomacy with little developmental value.
As one patient advocate notes:
“Nigeria is exporting its last doctors while patients queue at understaffed wards.”

Moving Forward: Balancing Diplomacy and Welfare
To redeem the TMA program, the Federal Government should:
- Harmonize expatriate and domestic pay.
- Fulfill previous welfare obligations: MRTF, hazard, and specialist allowances.
- Increase healthcare spending to meet AU benchmarks.
- Improve work environments and enhance retention through mentorship and infrastructure.
- Leverage diaspora experience in a way that builds domestic capacity.
Without these steps, the Saint Lucia agreement risks being perceived as cost-shifting diplomacy at Nigeria’s own expense.
At a moment when Nigeria’s health sector is in dire straits, the NMA’s criticism strikes at the heart of governance and ethics. Exporting doctors can signal global cooperation—but not if it abandons domestic duty. The coming 21-day ultimatum will test the government’s sincerity. And if ignored, Nigeria’s hospitals—and patients—may pay the price.
“There may be deeper political calculations behind this doctor-export deal — notably Nigeria’s strategic bid for Saint Lucia’s support in securing a seat at the United Nations Security Council. While diplomacy has its place, the Federal Government must not barter away national healthcare stability for geopolitical favors. Equalizing the pay and welfare of doctors at home with those sent abroad is the only way to avert a looming domestic collapse.”
— The National Patriots

Concrete, solution-oriented recommendations for the Nigerian Government to address the issues raised regarding the Nigeria- St. Lucia doctor deployment Deal and the Medical Workforce crisis.
Policy Recommendations: Five Steps to Fix the Crisis.
To ensure that Nigeria’s health diplomacy efforts, like the Saint Lucia agreement, serve both international interests and national welfare, the Federal Government must adopt a dual-focus approach—one that respects both global engagement and domestic priorities. The following are practical, strategic solutions:

Equalize Compensation and Welfare Standards
If Nigeria can pay doctors ₦40.8 million abroad, it should offer comparable packages at home to retain talent.
- Review and fully implement the CONMESS salary structure nationwide.
- Disburse the Medical Residency Training Fund (MRTF) promptly and transparently.
- Regularize hazard, rural service, and specialist allowances.
Declare a National Medical Workforce Emergency
- A Presidential Executive Order should recognize the ongoing brain drain as a national emergency and:
- Place a moratorium on the mass foreign deployment of doctors for at least 18 months.
- Set up a National Health Human Resources Taskforce to study and recommend reforms.
Upgrade Health Infrastructure and Working Conditions
- Doctors leave not only for money but also for modern tools, predictable power supply, secure workspaces, and career growth.
- Prioritize infrastructure investment in teaching hospitals, primary care centers, and rural health posts.
- Equip public hospitals with modern diagnostic tools, surgical suites, and life-saving equipment.
Create a Diaspora-Return Incentive Scheme
- Borrowing from models in India and Rwanda:
- Offer tax-free allowances, housing, and academic chairs to attract Nigerian doctors abroad for medium- to long-term service.
- Facilitate telemedicine partnerships and visiting lectureships for diaspora specialists.
Reform Medical Education and Career Progression
- Reduce bottlenecks in medical training and ensure that young doctors have a clear, achievable career path.
- Expand internship and residency slots in government-owned hospitals.
- Increase faculty funding and digital infrastructure for medical colleges.
- Allow private sector participation in residency and specialist training under NUC/NMDC supervision.

Notable Quote
> “A country that exports doctors while its own citizens die in waiting rooms must pause and rethink. Reform is not a luxury — it is a life-saving necessity.”
— Imran Khazaly.
Governance & Public Policy Analyst
Final Word
The Saint Lucia deal should not become a band-aid over a bleeding wound. Nigeria must treat the health sector with the urgency it accords defense and energy—or risk total collapse. What the NMA has raised is not opposition to diplomacy but a demand for domestic justice. Without robust reforms, the country may keep exporting its healers, while patients at home perish in silence.
> “The NMA should embrace dialogue in the spirit of the Hippocratic Oath to which all medical professionals are bound. A 21-day ultimatum risks being seen as confrontational without first formally seeking an audience with the Health Minister to present their case. Medical personnel are not labour agitators — they are guardians of life and must lead by example in seeking a peaceful, structured resolution.”
— Dr. G. Fraser, MFR
Governance & Perception Management Consultant
Filed by: Correspondent Emeka A. Obiora
For HeadlineNews.News